Menstrual Cycle 101

“It’s that time of the month” usually means one of two things: either rent is due, or someone’s menstrual period is here. Despite periods being one of the most common life experiences, there’s a lot that’s misunderstood. Let’s talk about why it happens once a month and how it relates to pregnancy.
What is the menstrual cycle?
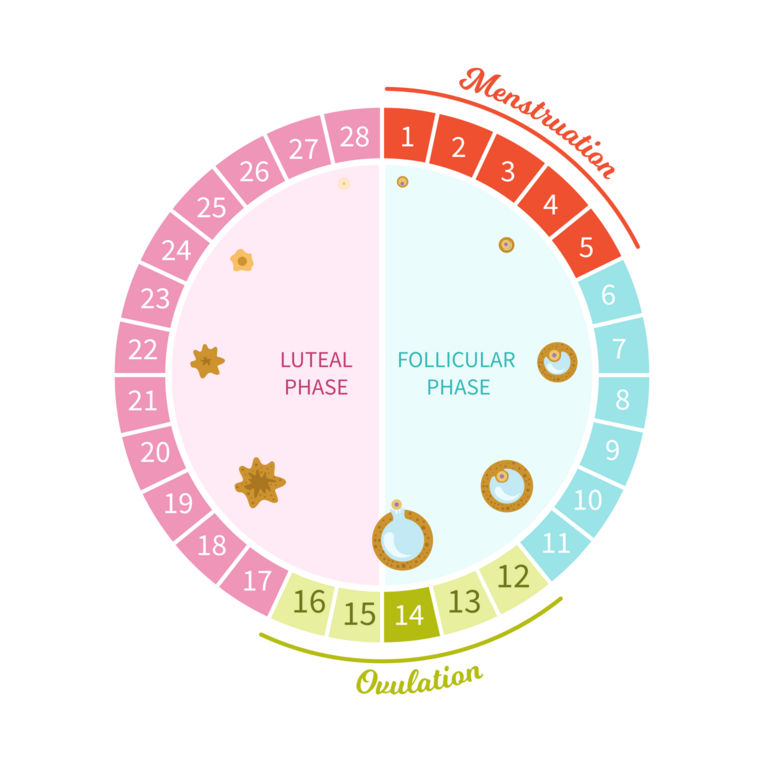
The menstrual cycle is a circular process with four phases that usually occur around once a month. It's the body's way of preparing for a pregnancy. It’s helpful to remember what is needed for a pregnancy: a sperm and an egg meet, combine, and implant in the uterus. The menstrual cycle is all about preparing the body for pregnancy–getting the egg ready, releasing it, and if there’s no pregnancy, starting all over again to try the next month. For most people, a menstrual cycle is around every 28 days, but could still be considered regular if it comes every 21-45 days. The first menstrual cycle could start as early as age eight (usually it starts around age 12) and ends with menopause in a person’s 40s or 50s. That’s a lot of cycles!
Four stages of the menstrual cycle
Menstruation: The first day of your period is the first day of the cycle. This typically lasts 3-7 days, and is when the lining of the uterus (the endometrium) is shed (this is the bleeding, or “period,” that you experience). The uterus may cramp during this time, causing pain or discomfort, as well as bloating and tiredness.
Follicular phase: This phase also begins on the first day of menstruation and continues for about 14 days. The body is using hormones to stimulate the ovaries to mature at least one egg. When the egg is ready, it will be released in hopes of meeting with a sperm to create a pregnancy. During this time, you may experience a heightened sex drive (libido) – this is the body’s way of encouraging pregnancy. By encouraging sexual activity, the body is increasing circumstances for sperm and the egg to come together. During this time, the body is also rebuilding the lining of the uterus to prepare for a fertilized egg.
Ovulation: There are thousands of follicles in the ovaries waiting to be developed into healthy eggs, but only one, sometimes two, are released during a typical cycle. When this egg is released, it is called ovulation. The egg will live in the body for 12-24 hours, traveling through the tubes from the ovary to the uterus to see if it meets with a sperm. (Note: some hormonal birth control methods stop ovulation from happening. No egg, no pregnancy!)
Luteal phase: This is the second half of the month-long cycle. This phase starts with ovulation, and ends when menstruation starts, usually around two weeks later. Often, hormones can rise and fall dramatically during this period, causing what some refer to as PMS or “premenstrual syndrome.” PMS may affect some people dramatically, and others not at all. Common symptoms could include bloating, anxiety or mood changes, tiredness, and other physical discomfort. During the luteal phase, if no pregnancy has occurred, the uterus will shed that lining it had built up so hopefully earlier in the month–beginning the cycle all over again with menstruation. If the sperm and egg have met, it’s possible that the fertilized egg could implant in the uterus, leading to pregnancy.
Follicular phase: This phase also begins on the first day of menstruation and continues for about 14 days. The body is using hormones to stimulate the ovaries to mature at least one egg. When the egg is ready, it will be released in hopes of meeting with a sperm to create a pregnancy. During this time, you may experience a heightened sex drive (libido) – this is the body’s way of encouraging pregnancy. By encouraging sexual activity, the body is increasing circumstances for sperm and the egg to come together. During this time, the body is also rebuilding the lining of the uterus to prepare for a fertilized egg.
Ovulation: There are thousands of follicles in the ovaries waiting to be developed into healthy eggs, but only one, sometimes two, are released during a typical cycle. When this egg is released, it is called ovulation. The egg will live in the body for 12-24 hours, traveling through the tubes from the ovary to the uterus to see if it meets with a sperm. (Note: some hormonal birth control methods stop ovulation from happening. No egg, no pregnancy!)
Luteal phase: This is the second half of the month-long cycle. This phase starts with ovulation, and ends when menstruation starts, usually around two weeks later. Often, hormones can rise and fall dramatically during this period, causing what some refer to as PMS or “premenstrual syndrome.” PMS may affect some people dramatically, and others not at all. Common symptoms could include bloating, anxiety or mood changes, tiredness, and other physical discomfort. During the luteal phase, if no pregnancy has occurred, the uterus will shed that lining it had built up so hopefully earlier in the month–beginning the cycle all over again with menstruation. If the sperm and egg have met, it’s possible that the fertilized egg could implant in the uterus, leading to pregnancy.
What does all this mean for pregnancy risk?
The reality is, it will depend from person to person. Generally speaking, people are at less risk for pregnancy after ovulation and before menstruation. At this time, the egg that was released has likely dissolved and no new eggs are available. The trouble is that most people don’t know when they ovulate. A longer cycle one month and a shorter cycle the next month can drastically impact pregnancy risk, meaning most people don't know where they are in their cycle on any given day.
Tracking your cycle to avoid pregnancy can be difficult. Another challenge is with those who have irregular periods. What is described above is a “normal” cycle. Unfortunately, people’s cycles can change based on stress, nutrition, physical activity, age, hormones, environment, or medical conditions. Someone’s cycle as a teenager may be different than their cycle approaching menopause, and especially in someone who recently had a baby or is breastfeeding. Those differences come with real changes in pregnancy risk. Even for people with normal cycles, relying only on cycle tracking for pregnancy prevention varies greatly. To be safer, consider using condoms and/or a prescription method of birth control. Learn more here!
Tracking your cycle to avoid pregnancy can be difficult. Another challenge is with those who have irregular periods. What is described above is a “normal” cycle. Unfortunately, people’s cycles can change based on stress, nutrition, physical activity, age, hormones, environment, or medical conditions. Someone’s cycle as a teenager may be different than their cycle approaching menopause, and especially in someone who recently had a baby or is breastfeeding. Those differences come with real changes in pregnancy risk. Even for people with normal cycles, relying only on cycle tracking for pregnancy prevention varies greatly. To be safer, consider using condoms and/or a prescription method of birth control. Learn more here!
Resources
For more resources about tracking menstrual cycles, check out the Office on Women’s Health and Planned Parenthood.
